

Dysphagia is often due to mechanical obstruction of the food passage, which can be due to recurrent or acutely developing gastric or esophageal obstruction. This is more pronounced with solid foods than with liquids. The paraesophageal hernias are more commonly associated with difficulty in swallowing ( dysphagia). Prolonged or severe upper gastrointestinal bleeding can lead to anemia. The lining of the stomach (gastric mucosa) can sustain ischemic injury in following such events and may result in bleeding. The herniated organs can result in abdominal or chest pain (epigastric and retrosternal) due to torsion or distension. Some patients with large paraesophageal hernias can also develop respiratory symptoms like cough, wheezing and is often associated with laryngopharyngeal reflux ( LPR Reflux). With progression of the hernia, the regurgitation becomes severe, even reaching stages where a person may be unable to bend without experiencing regurgitation.ĭiscoloration of the teeth (yellowing teeth) may be seen in patients with severe long standing GERD with regurgitation of gastric contents into their mouth. The onset of regurgitation indicates an enlarging hiatal hernia. Symptoms usually start with heartburn and slowly progress to regurgitation of digested food. GERD usually presents with chronic heartburn but other symptoms like nausea and excessive belching may also be present. Small hernias, especially small sliding hernias, are less frequently associated with reflux but the risk of GERD increases with size of the hernia. However, most patients with a sliding hiatal hernia (type I) and paraesophageal/rolling hernia (type II) have associated gastroesopageal reflux disease ( GERD).
Typical symptoms of a hiatal hernia includes heartburn, regurgitation, abdominal and chest pain and chronic nausea. Many hiatal hernia cases are asymptomatic meaning that a person does not experience any symptoms.
#Type 3 hiatal hernia free#
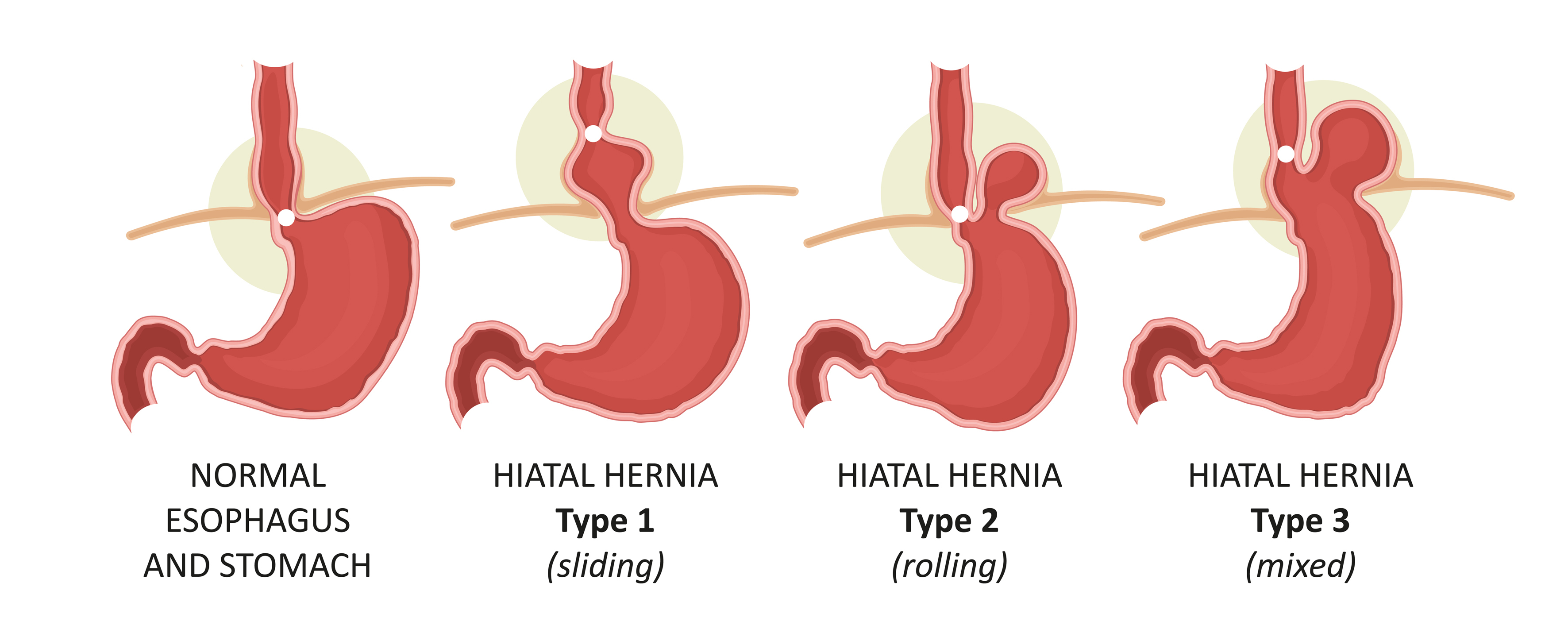
In the type III hiatal hernia the gastroesophageal junction can slide into the thorax and the fundus of the stomach (or colon) is free to roll into the thorax. Mixed hiatal herniaĪ type III hiatal hernia is a paraesophageal hernia having combined features of sliding and rolling hiatal hernia. Rarely part of the colon or the spleen may pass through the hiatal defect.
The thorax has a negative pressure compared to the abdominal cavity, and this facilitates the abdominal visceral herniation (protrusion) into thorax. The gastroesophageal junction remains fixed at the normal position in the abdomen, but hiatal defect allows protrusion of abdominal viscera into thorax.Ī part of the stomach (usually the fundus) herniates through the defect and remains by the side of esophagus. The defects in type II hiatal hernias are usually large. Rolling hiatal herniaĪ olling hiatal hernia (type II) is a type of paraesophageal hernia and accounts for 4% to 5% of hiatal hernias. The risk of reflux increases with the size of the hernia.

This allows for the back flow of the stomach contents into the esophagus ( acid reflux). This, along with the negative pressure in the thoracic cavity can result in weakening of lower esophageal sphincter (LES). In a sliding hiatal hernia, the gastroesophageal junction is not maintained in the abdominal cavity but is allowed to move back and forth (slide) between the thoracic and abdominal cavity. Type II or rolling hiatal hernia or paraesophageal hiatal herniaĪ sliding hiatal hernia (type I) is the most common type, accounting for about 95% of cases.There are broadly two types of hiatal hernias, a sliding or rolling hiatal hernia, but is possible to have a mixed type which is a combination of a sliding and rolling hiatal hernia. Many hiatal hernia cases are silent (asymptomatic). The incidence of a hiatal hernia increases with age and it is fairly prevalent in the over 50 age group. A hiatal hernia, also known as a hiatus hernia, is the abnormal protrusion of the upper part of the stomach into the thoracic cavity through a defect in the diaphragm.


 0 kommentar(er)
0 kommentar(er)
